What is sleep paralysis
What is sleep paralysis
Causes and Risk Factors of Sleep Paralysis
Triggers Include Sleep Deprivation, Narcolepsy, and Sleep Apnea
Sleep paralysis is a relatively common experience—about 8% of people will experience it at one point or another, with higher rates for students, people of color, and people with psychiatric conditions.
It occurs when the features of rapid eye movement (REM) sleep intrude into wakefulness, leading to muscles that are unable to move, impaired breathing, and features of vivid dreams like fear and hallucinations. This disconnect between the brain and the body’s muscles can cause terrifying symptoms.
What are the causes of sleep paralysis? Are there things you can do to avoid experiencing it?
There may be some factors that play into sleep paralysis that are beyond your control, but some self-induced behaviors may potentially trigger an episode of sleep paralysis in the right situation. By learning how certain causes can potentially lead to sleep paralysis, you may be better able to avoid it.
Definition
Sleep paralysis is simply an extension of the dream state (called REM or rapid eye movement sleep), so it is technically harmless. However, it is not something people seek to repeat once they experience it, as it can be unpleasant.
People experience an inability to move, speak, or control their body, despite being conscious and wanting to. It is sometimes accompanied by hallucinations, which add to the disagreeable nature of the situation.
Causes
The causes of sleep paralysis are surprisingly mundane. Consider the two states of consciousness—being asleep and being awake. There is normally a transition period between these states.
During this transition, elements of consciousness—such as an awareness of your environment—may be preserved, while aspects of sleep (such as dreaming) may begin. Typically, this transition is brief and uneventful. However, a prolonged or disrupted transition may predispose you to the unusual experiences of sleep paralysis.
REM Sleep Problems
In particular, sleep paralysis is believed to relate to a problem regulating REM sleep. It is during REM that our body is paralyzed so that we are unable to act dreams out.
This muscle relaxation, called atonia, may sometimes occur while you are awake. As such, you will be unable to move, even if you are conscious. This is one of the common features of sleep paralysis.
Clearly, there are certain triggers of sleep paralysis. It often occurs during periods of sleep deprivation and stress. Many people experience it when their sleep schedule is disrupted, no matter the reason.
Those with shift work sleep disorder may be at increased risk, according to a 2016 review study. If sleep is attempted during the day, it is more likely for interruptions of sleep to occur.
In addition, it is possible to trigger sleep paralysis experimentally by disrupting REM. In a controlled environment (such as a sleep study), this could be attempted—and has been shown to incite the phenomenon.
Psychiatric Disorders
There also appears to be a strong association with psychiatric disorders like anxiety and depression. The use of alcohol or other drugs may also provoke an attack of sleep paralysis. For some people, a family history of sleep paralysis becomes evident, though a genetic cause of the condition is not known.
Sleeping Position
Most people with sleep paralysis report that it occurs when they are sleeping on their backs (a supine sleeping position). However, less frequently, others have reported it occurring when sleeping on their stomachs or sides as well.
Timing
The vast majority of people suggest that sleep paralysis happens while falling to sleep (a hypnagogic phenomenon), yet it can also occur when awakening from sleep. It typically occurs at night, but it has also been known to occur during daytime naps.
Other Sleep Disorders
Sleep paralysis can also occur in association with other sleep disorders that fragment sleep, including obstructive sleep apnea and narcolepsy. Sleep apnea is often worsened by being on one’s back and in REM sleep, so other symptoms such as snoring and waking to urinate may suggest a need for testing.
Symptom of narcolepsy include sleepiness, hallucinations, and cataplexy (sudden and transient loss of muscle tone). Treatment of these conditions may reduce the frequency of sleep paralysis episodes.
Unscientific Explanations
Sleep paralysis has occurred throughout recorded history, and there are countless examples in literature and art of the phenomenon. In some parts of the world, the condition is called the «old hag.»
Religion
Many people describe the experience in religious terms. Some might blame a ghost, demon or devil as the cause. The terrifying elements of sleep paralysis are easily ascribed to a malevolent presence. Others suggest it is due to aliens. There is no scientific evidence for such beliefs.
Medical and Mental Problems
Others worry that another medical or mental health problem may be to blame. The list of potential medical maladies that might explain the experience of sleep paralysis is diverse, ranging from seizures to heart attacks to strokes. Some even think (at least briefly) that they have died.
Still, other people worry that they have gone insane and do not discuss it because they are worried about how others might react to their experience. The episode of sleep paralysis is self-limited, without lasting consequences, and so these explanations are proven to be false.
Dreams and Nightmares
Finally, some people worry that sleep paralysis is just a dream or a nightmare. This may actually be the closest to the truth. As described above, sleep paralysis occurs when there is a breakdown between the states of consciousness and sleep, when our dream state intrudes upon our wakefulness.
Fortunately, many people are reassured by a better understanding of the phenomenon of sleep paralysis, so that if it recurs they know how to interpret the experience and can more easily tolerate it until it inevitably ends.
A Word From Verywell
For most people, sleep paralysis occurs rarely, but if it occurs more frequently and you find it particularly bothersome, you may wish to speak to your healthcare provider for a referral to a board-certified sleep medicine healthcare provider. Treatment of narcolepsy or sleep apnea, if present, may be helpful.
Even if your sleep paralysis occurs in isolation, if it has become disruptive to your life, treatment options are available.
Sleep Paralysis
Articles On What Is Sleep Paralysis?
Is Sleep Paralysis a Symptom of a Serious Problem?
Sleep researchers conclude that, in most cases, sleep paralysis is simply a sign that your body is not moving smoothly through the stages of sleep. Rarely is sleep paralysis linked to deep underlying psychiatric problems.
Over the centuries, symptoms of sleep paralysis have been described in many ways and often attributed to an «evil» presence: unseen night demons in ancient times, the old hag in Shakespeare’s Romeo and Juliet, and alien abductors. Almost every culture throughout history has had stories of shadowy evil creatures that terrify helpless humans at night. People have long sought explanations for this mysterious sleep-time paralysis and the accompanying feelings of terror.
What Is Sleep Paralysis?
Sleep paralysis is a feeling of being conscious but unable to move. It occurs when a person passes between stages of wakefulness and sleep. During these transitions, you may be unable to move or speak for a few seconds up to a few minutes. Some people may also feel pressure or a sense of choking. Sleep paralysis may accompany other sleep disorders such as narcolepsy. Narcolepsy is an overpowering need to sleep caused by a problem with the brain’s ability to regulate sleep.
When Does Sleep Paralysis Usually Occur?
Sleep paralysis usually occurs at one of two times. If it occurs while you are falling asleep, it’s called hypnagogic or predormital sleep paralysis. If it happens as you are waking up, it’s called hypnopompic or postdormital sleep paralysis.
What Happens With Hypnagogic Sleep Paralysis?
As you fall asleep, your body slowly relaxes. Usually you become less aware, so you do not notice the change. However, if you remain or become aware while falling asleep, you may notice that you cannot move or speak.
What Happens With Hypnopompic Sleep Paralysis?
During sleep, your body alternates between REM (rapid eye movement) and NREM (non-rapid eye movement) sleep. One cycle of REM and NREM sleep lasts about 90 minutes. NREM sleep occurs first and takes up to 75% of your overall sleep time. During NREM sleep, your body relaxes and restores itself. At the end of NREM, your sleep shifts to REM. Your eyes move quickly and dreams occur, but the rest of your body remains very relaxed. Your muscles are «turned off» during REM sleep. If you become aware before the REM cycle has finished, you may notice that you cannot move or speak.
Who Develops Sleep Paralysis?
Up to as many as four out of every 10 people may have sleep paralysis. This common condition is often first noticed in the teen years. But men and women of any age can have it. Sleep paralysis may run in families. Other factors that may be linked to sleep paralysis include:
How Is Sleep Paralysis Diagnosed?
If you find yourself unable to move or speak for a few seconds or minutes when falling asleep or waking up, then it is likely you have isolated recurrent sleep paralysis. Often there is no need to treat this condition.
Check with your doctor if you have any of these concerns:
Your doctor may want to gather more information about your sleep health by doing any of the following:
How Is Sleep Paralysis Treated?
Most people need no treatment for sleep paralysis. Treating any underlying conditions such as narcolepsy may help if you are anxious or unable to sleep well. These treatments may include the following:
What Can I Do About Sleep Paralysis?
Show Sources
American Academy of Sleep Medicine: «Sleep Paralysis.»
National Sleep Foundation: «Ask the Sleep Expert: Sleep & Parasomnias;» «Sleep Paralysis;» «Topics A to ZZZZs: Narcolepsy;» and «What Happens When You Sleep?»
What Is Sleep Paralysis?
Caitilin Kelly, MD, is a clinical physician at Indiana University Health Bloomington Hospital and is board-certified in internal medicine.
Sleep paralysis is when you’re temporarily unable to move or speak as you go from sleep to wakefulness, or vice versa. It can last seconds to minutes, during which time you may feel like you are touching, hearing, smelling, or seeing people or things that aren’t really there.
You may feel anxious, scared, or even like you’re going to die (or that you’re already dead). You are aware of the experience, but unable to do anything to control it.
Luckily, most people who experience sleep paralysis don’t typically have it often. When they do, the cause is usually relatively harmless with no serious risks. However, some conditions that can affect your health may be to blame.
Here’s everything you need to know about sleep paralysis, including what causes it and what you can do if it happens to you.
Sleep Paralysis Symptoms
Sleep paralysis can occur when you’re waking up, or what’s called a hypnopompic state. It can also happen when you’re falling asleep, or in a hypnagogic state. The latter is more common in people with narcolepsy, a sleep disorder that makes you sleep too much.
You’re more likely to experience sleep paralysis closer to the morning. That’s when rapid eye movement (REM), the sleep stage associated with vivid dreaming, occurs. It also happens more often when you sleep on your back.
Common features of sleep paralysis include:
For example, you may feel like someone is standing over you. You try to move your head to look, but you can’t. It feels like someone—or something—is holding you down. You feel like you can’t breathe.
You may try to thrash your arms and legs, but you’re frozen in place. Sheer panic washes over you. You may even fear like your life is in danger.
While many people have scary sensations, it’s also possible to have pleasant ones.
Recap
Common symptoms of sleep paralysis are the feeling that you’re not able to move or speak, the presence of something or someone else in the room, hearing noises or voices that aren’t there, or feeling like someone is touching you.
Prevalence
Sleep paralysis usually happens to people in their 20s and 30s, but some have their first episode as teenagers.
People with certain medical or mental health conditions—like narcolepsy or sleep apnea—are more likely to have sleep paralysis.
Sleep paralysis has a strong genetic component and may run in families, according to a 2011 review of several studies.
Sleep paralysis is relatively common. A 2011 review reported that about 7% of people experienced sleep paralysis at least once.
The study also noted that it affects some people more than others. For example, 28% of students and 34% of people with panic disorder have reported episodes of sleep paralysis.
A 2018 study found that student-athletes regularly reported sleep paralysis. The study also found students with depression had higher instances of sleep paralysis.
Causes
Sleep deprivation, stress, and a disrupted sleep schedule can trigger sleep paralysis.
Anxiety disorders also have a strong link, likely because they lead to insomnia or lighter, fragmented sleep.
A 2016 review found that sleep paralysis occurs with disruption of rapid eye movement (REM), or dream sleep. Although specific triggers play a role, some people believe it’s related to a problem with REM regulation. During this phase of sleep, your body relaxes so that it doesn’t physically act out dreams.
This type of relaxation can cause temporary paralysis if it happens while a person is awake. Other elements of vivid dream sleep can continue as you wake up and also occur with disrupted REM.
Obstructive sleep apnea can disrupt your breathing. This causes you to wake up throughout the night, resulting in an episode of sleep paralysis. This explains why someone who sleeps on their back is more likely to have sleep paralysis.
Your condition may have an underlying cause, such as sleep apnea if you have symptoms like:
In rare cases, another disorder mimics sleep paralysis. One example is a focal epileptic seizure. A video electroencephalogram (EEG) can help differentiate between the two. An EEG is a test that records your brain’s electrical activity.
Recap
A disruption in REM sleep (deep, rapid eye movement sleep) is the cause of sleep paralysis in most cases. But if you have other symptoms, too, it can be a sign of a related condition, like sleep apnea, anxiety disorder, or narcolepsy.
Treatment
Sleep paralysis ends within a few minutes, either when you go back to sleep or fully wake up. Treatment is not typically needed and most people feel like they can cope after they know they’re not actually in danger.
If you’re prone to episodes of sleep paralysis, improving your sleep hygiene can often help. While it sounds like a sleepy shower, sleep hygiene actually refers to healthy habits that help you fall into a deep sleep. Some of these include:
In rare cases, people suffer from repeated episodes and feel like they can’t handle the psychological distress.
Medicine that suppresses the REM cycle of sleep sometimes helps. This includes selective serotonin receptor inhibitors (SSRIs) and tricyclic antidepressants (TCAs).
Ask your healthcare provider to evaluate you to address any sleep, mental health, or other medical disorders that can disrupt sleep, like sleep apnea or narcolepsy.
If you have multiple or recurring episodes of sleep paralysis and these strategies don’t help, your healthcare provider might refer you to a board-certified sleep specialist for an evaluation that will likely include a sleep study.
Coping
Some people find that mindfulness meditation and muscle relaxation exercises help them cope with sleep paralysis.
When you experience sleep paralysis, focus on relaxing your mind. Tell yourself that:
Some people even like to engage in the experience. They’ll pretend they’re an actor in a scary movie. This gives them a sense of control over something that otherwise makes them feel powerless.
If you can reassure and distract yourself enough to fall back asleep, the experience will quickly end.
Recap
If sleep paralysis often happens to you, there are ways you can learn to cope with it. First, rest assured that it’s usually harmless. Focus on improving your sleep habits, practice mindfulness exercises, or even pretend you’re in a scary movie and engage in the experience.
Summary
Sleep paralysis is somewhat common in adults but especially affects students and people with panic disorders. It happens when the transition to sleep or awakening is disrupted, and there’s an interruption in your REM sleep.
Many times people experience hallucinations that they can see, hear, smell, or feel. Most people don’t like the experience and often feel scared. But usually, sleep paralysis is harmless.
If it’s really bothering you or if you have other symptoms of sleep disorders, see your healthcare provider or a sleep specialist.
Frequently Asked Questions
You might be experiencing hypnopompic paralysis. It happens as your brain transitions from sleep to waking up, or the other way around. Get enough rest and treat any underlying anxiety to keep it from repeating. You have nothing to worry about if it doesn’t happen often, but talk to your healthcare provider if it does.
Yes. Without enough sleep, your brain doesn’t function as well. You might see, feel, hear, smell, or even taste things that aren’t there. Some people have these hallucinations right after they wake up or when they fall asleep after a long period of not getting enough sleep.
What Are the Symptoms of Sleep Paralysis?
Inability to speak or move, hallucinations, and fear
Kashif J. Piracha, MD, is board-certified in internal medicine and nephrology. He has an active clinical practice at Methodist Willowbrook Hospital in Houston, Texas.
Sleep paralysis symptoms include hallucinations, feeling afraid, and the sensation that you can’t move or speak. These episodes can happen when the transition between rapid eye movement (REM) sleep and waking up is disrupted.
This article goes over common sleep paralysis symptoms.
» data-caption=»» data-expand=»300″ data-tracking-container=»true» />
Verywell / Brianna Gilmartin
Sleep Paralysis Symptoms
Symptoms of sleep paralysis include:
These symptoms often last for several minutes.
They occur because, during REM sleep, the diaphragm (a large muscle below your lungs involved with your breathing) acts as a bellows to help you inflate your lungs and breathe. While the diaphragm is active, other breathing muscles (like around the rib cage) aren’t as active. That’s what causes these symptoms.
The level of awareness during sleep paralysis varies. Some people claim they’re completely awake and aware of their surroundings. Others describe only partial awareness.
Sleep Paralysis Hallucinations
You may also experience vivid hallucinations during sleep paralysis. With these, you feel like you are experiencing something that isn’t not actually occurring—like you’re dreaming while awake.
The hallucinations linked to sleep paralysis fall into four categories based on the senses they affect:
Visual Hallucinations
Symptoms of visual hallucinations can include seeing:
Sometimes the visual hallucination can be really detailed. For example, some have reported seeing a hand not attached to a body, a gargoyle, bugs, or even a cat.
In other cases, people have vague visions that are blurry or shimmering. They might also have a sense that things in the room are floating.
Auditory Hallucinations
Similarly, the auditory (hearing) hallucinations in sleep paralysis can range from routine to bizarre.
Many people hear various noises, but hearing voices is the most common. The voices may sound like whispers, screams, or laughter.
Almost as often, people report hearing a loud buzzing or static noise. It sounds like a radio that’s on but not tuned to a station. Some people hear breathing, footsteps, knocking, or a ringing sound.
People might hear unusual sounds like a horse carriage or growling.
The sounds heard aren’t always specific. They can be hard to describe or remember.
Recap
During sleep paralysis, you might think you see something that isn’t actually there. Sometimes it looks like a person, animal, or even an odd figure. You might also see flashes of color or light, or hear unusual noises like a buzzing or growling.
Tactile Hallucinations
Tactile hallucination is the experience of being touched when you’re not. It’s one of the most common aspects of sleep paralysis. Many people say they feel pressure or contact. It’s like something or someone is holding them down.
Some people with sleep paralysis report tingling, numbness, or a vibrating sensation. Others describe a sense of floating, flying, or falling. A few people report feeling chilled or freezing.
Less often, people feel like they’re being physically moved or dragged from their beds. Some people report feelings of sexual contact, including physical sensations involving their genital areas.
Other physical experiences that people have reported include:
Olfactory Hallucinations
The least common hallucination in sleep paralysis is olfactory (sense of smell). Like the other types of hallucinations, the intensity of the smells ranges.
Recap
During sleep paralysis, you might smell things that aren’t there or feel like someone or something is touching you when it’s not.
Emotional Symptoms
An important and lasting element of sleep paralysis is the emotional component.
For many, the experience of sleep paralysis is a waking nightmare. The dark figure you sense in the room seems to be an evil presence, intent on real harm. The stranger standing over you or sitting on top of you is up to no good, and so on.
Most people who experience sleep paralysis describe it as a scary, terrifying, horrifying, or frightening experience. This is often related to the hallucination of a stranger’s presence. Some people have a sense of impending doom, or the feeling that real harm or death is about to happen to them.
When you first experience sleep paralysis, it may feel like you had a stroke that resulted in locked-in syndrome. With this, you’re conscious but unable to move anything except for your eyes.
Many people describe how real everything seems when it’s happening. It’s common for people to use the words «weird» and «strange» to describe their experiences.
People might summarize their sleep paralysis as shocking, worrisome, or disgusting. They may say it left them scared, angry, or helpless. Rarely, the experience actually feels comforting to some people.
It may be helpful to have a better understanding of the symptoms of sleep paralysis. Knowing what’s happening to you may give you comfort. For some people, it’s enough to tolerate these infrequent episodes.
For others, this information can help end triggers of sleep paralysis. If these episodes are especially disturbing to you, there are effective treatment options.
Causes of Sleep Paralysis
First, it’s important to understand what sleep paralysis is. It’s the presence or persistence of features of REM sleep during the transition into or out of sleep.
It can take place when you’re first falling asleep ( hypnagogic state). But it can also occur when you’re waking up ( hypnopompic state).
About 20% of healthy people experience sleep paralysis. Most people with sleep paralysis experience it without any related conditions. But it can happen along with other symptoms if you have narcolepsy, a sleep disorder that causes excessive sleepiness.
During REM, your mind is active. You might vividly imagine sights, sounds, and other feelings as part of a dream. You might even feel afraid like you would in a nightmare.
At the same time, your body is paralyzed so you can’t act out your dreams. This is called muscle relaxation or atonia. When these features happen during wakefulness, you’re experiencing sleep paralysis.
Recap
Normally, you have a smooth transitions between the different phases of sleep. But when a transition is interrupted, you might experience sleep paralysis. This can happen either when you first fall asleep or when you’re about to wake up.
Summary
Sleep paralysis happens when there’s a glitch in your sleep, usually between REM sleep and waking up.
During sleep paralysis, you might hallucinate and think you’re seeing, hearing, smelling, or feeling something that’s isn’t actually there.
It can be a scary feeling, but it’s usually not a sign of anything serious.
A Word From Verywell
Sleep paralysis doesn’t always happen often. Once you understand what it is and why it happens, you might forget about it. If it doesn’t go away, consider ways to optimize your sleep. Make sure you’re getting enough sleep with a regular sleep pattern. Avoid alcohol in the hours before bedtime. It may also be helpful to try to sleep on your sides as much as possible.
In some cases, you might have to do a sleep study. This could find other factors that cause sleep fragmentation, like sleep apnea. If you need help, talk to a board-certified sleep doctor about your concerns.
What is Sleep Paralysis?
Dr. Colleen Ehrnstrom, Ph.D., ABPP
Colleen Ehrnstrom, Ph.D., ABPP, is a licensed clinical psychologist. She specializes in acceptance and commitment therapy (ACT) and is board certified in cognitive behavioral therapy (CBT). At the University of C.
Eachnight may earn commissions for products you purchase through our links. Our articles and reviews include affiliate links and advertisements, including amerisleep advertising. Learn more
If you suffer from sleep paralysis, then you’re probably familiar with hearing or seeing things that aren’t there while you sleep, or worse, feeling like you can’t move or run away from your own imagination. Don’t worry—what you’re experiencing lasts no longer than a few minutes, and many others encounter the same phenomenon. Sleep paralysis is often caused by stress or sleep deprivation. All across the world, people experience sleep paralysis and have had wide-ranging theories about its causes and underlying meaning.
This article discusses what sleep paralysis is, what it feels like to undergo an episode, symptoms leading to a diagnosis, and who is at risk. We will also explore the causes of sleep paralysis and how to prevent the disorder.
But What Is Sleep Paralysis?
Sleep paralysis, or sleep atonia, is a term used to describe a sleep disorder in the class known as parasomnia disorders. It is an episodic event that happens during your sleep cycle that typically involves temporary paralysis and/or difficulty breathing, hallucinations, and feelings of fear. Atonia literally means loss of muscle movement; however, in the case of sleep paralysis, you haven’t lost muscle movement; rather the mechanics of your sleep cycle temporarily stops the muscle movement from happening.
Sleep paralysis is a normal part of REM sleep. However, it is considered to be a disorder when it occurs outside of REM sleep. It can occur in otherwise healthy people, as well as in those presenting symptoms of narcolepsy, cataplexy, and hypnagogic hallucinations.
Interesting Fact: REM sleep is the stage of sleep that increases in duration throughout the night and, therefore, dominates the second half of a person’s nighttime sleep cycle. It is characterized by rapid eye movement and dreaming. The body’s heart rate increases and breathing becomes short and shallow. Brainstem neurons communicate differently with the body during the REM sleep stage which reduces body movement, preventing you from acting out your dreams.
What Sleep Paralysis Feels Like
Sleep paralysis is experienced differently from person to person; however, its core symptoms are consistent for most people.
During sleep paralysis episodes, you cannot speak or move, as your body is in a physiological state that prohibits movement even though your mind is awake. Being aware or awake when your body is unable to move can naturally cause you to hyperventilate and hallucinate.
Sleepers who experience these episodes can hear sounds or smell odors. Oftentimes, these hallucinations have a sinister context, such as approaching footsteps or smell odors akin to something decomposing.
If you find yourself in one of these episodes, remember, sleep paralysis is temporary and lasts no more than a few minutes.
Who’s at Risk
About 8-10% of the population experiences sleep paralysis. Most cases appear during your teen years, although it can occur at any age. It can run in families and is not correlated with other health concerns. Sleep paralysis is also often triggered by stress and trauma.
Traumatic Life Events
A medical paper discusses how panic disorders and post-traumatic stress disorder (PTSD) increase the risk of sleep paralysis due to higher physiological distress.
A study conducted with Cambodian refugees showed a significant connection between traumatic life events and increased chance of sleep paralysis. The researchers reported that almost half of the refugees suffered at least one sleep paralysis attack within the prior 12 months. Similarly, people with clinically diagnosed PTSD had increased risk – almost four times more than people who do not have PTSD.
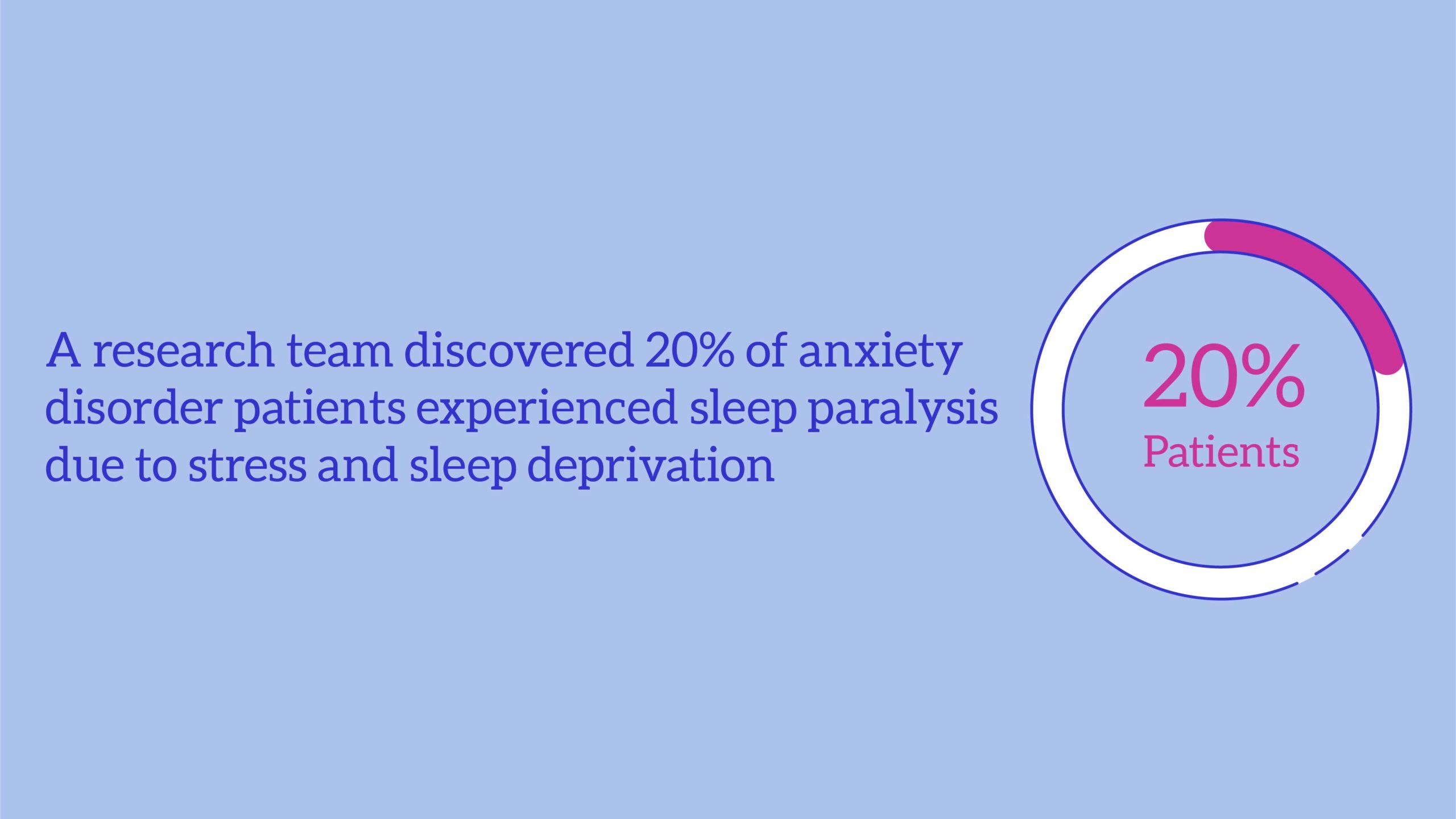
Psychological Disorders
Studies in the past few decades have shown that 20% of people with a diagnosed anxiety disorder experienced sleep paralysis. This is often thought to be due to increased levels of stress and sleep deprivation.
More specifically, people with social anxiety who also have sleep paralysis experience extreme distress levels, including anxiety, feelings of being observed, and fears of death in non-threatening situations.
Canadian researchers Sigmar and Nielsen looked deeper into the connection between social anxiety, sleep paralysis, and depression. They found sleep paralysis sufferers with sensed presence symptoms often also had high levels of social anxiety. The scientists have theorized that people with social anxiety generate threatening hallucinations of a harmful presence during sleep paralysis and these hallucinatory images may stem from past trauma.
Researchers in the U.S. Szklo-Coxe, Young, Finn, and Mignot found that depression is strongly associated with sleep disturbances and sleep paralysis. The study showed that sleep paralysis was not associated or caused by other possible factors, such as use of antidepressants, daytime sleepiness, and insomnia. This leads to the conclusion that depression is a separate risk factor from anxiety for sleep paralysis.
Sleep Paralysis Symptoms
Shelley Adler’s book Sleep Paralysis: Night-Mares, Nocebos, and the Mind-Body Connection list a collection of symptoms. Someone doesn’t need to endure all of these symptoms to have a sleep paralysis episode—only three of them need to occur to meet the criteria.
Awareness or Sense of Being Awake
Most people feel consciously awake as they experience sleep paralysis. You are awake and aware of the area around your bed and distinctive elements, such as furniture and others in the room.
Inability to Move
Aside from realizing they’re awake, body paralysis is the first element noticed by the affected person. The paralysis stems from the body remaining in REM sleep when brainstem neurons don’t communicate with the body. Body immobility prevents them from acting out their dreams, which keeps them from sustaining injuries in their sleep.
During sleep atonia, sleepers can often erroneously assume the state of paralysis is due to an outside force, either holding the sleeper down or sitting on them.
Overwhelming Fear and Dread
People often feel afraid during a sleep paralysis episode. The fear can stem from realizing they are immobile or another symptom of sleep atonia.
Sometimes these feelings are too intense, and people struggle to comprehend them. These feelings of fear may follow individuals into wakefulness and progress into a sense of foreboding connected to sleep.
Sense of Presence
Some people may sense or see a “presence” in the room with them. If seen, the presence can take the appearance of a shadowy human-like creature standing near the bedside or sitting on top of the sleeper.
Difficulty Breathing
Pressure on the chest is a common sensation associated with sleep paralysis. The sensation is due to the body adopting a shallow breathing pattern needed for REM sleep.
Many people report they experience difficulty breathing due to the “presence” in their bedroom sitting on their chest or restricting their airways.
Supine Position
Most episodes of sleep paralysis happen while the individual is lying on their back. We don’t know why lying on the back increases the risk of sleep paralysis, though.
Unusual Sensations
People commonly report hallucinations accompanied by auditory, olfactory, and physical symptoms.
Individuals said they heard the sound of doors opening and closing, animal growls, footsteps, scratching, beeping or buzzing, whisperings of malevolent intent. People can smell dampness, mold, and feel as though they are drifting, rolling, floating, and being moved. Other people report out-of-body experiences.
Prevention and Treatments
Skip nap time. Sleep specialist Clete Kushida, MD, Ph.D., says, “nappers seem more prone to sleep paralysis than non-nappers.”
Get as much sleep as possible. Sleep-deprived individuals have a higher sleep paralysis risk. Putting yourself on a sleep schedule can help to prevent you from staying up too late and ensures you will get 7 to 9 hours of sleep.
Practice good sleep hygiene or sleep habits. Sometimes sleep disturbances are caused by a poor bedtime routine and sleep environment. Other times, you can improve your sleep quality by adding a few relaxing bedtime rituals:
Don’t sleep on your back. Sleep experts found sleeping on your back can cause more instances of sleep paralysis. Besides, side sleeping opens the airways to reduce sleep apnea symptoms and reduces instances of sleep atonia. Dr. Ehrnstrom notes, “It can be helpful to tape a tennis ball to your nightclothes to help train your body to sleep on your side.”
Seek a physician’s help. Sleep paralysis is sometimes linked to other sleep disorders: sleep apnea, narcolepsy, insomnia, or sleep deprivation. If sleep paralysis episodes often occur, see a sleep specialist. If you’re dealing with high levels of anxiety, we suggest speaking with a psychiatrist about your worries.
Frequently Asked Questions
What triggers sleep paralysis?
Stress, sleep deprivation, jet lag, and an inconsistent sleep schedule can trigger sleep paralysis. Sleep paralysis does occur most commonly during adolescence, and if you’re somebody younger who experiences sleep paralysis, it may have more to do with puberty than with actual triggers. However, if you’re in your teens and older, there may be an underlying cause of sleep paralysis.
Why is sleep paralysis so scary?
Sleep paralysis is especially alarming because it immobilizes you, and if you’ve never experienced sleep paralysis before, the feeling of being unable to move is particularly scary. Plus, many hallucinate or see “figures” during sleep paralysis episodes—and unknown shadowy figures are bound to scare anybody. (Don’t worry, though, they’re not real!)
Can someone wake you up during sleep paralysis?
Someone may be able to somewhat wake you, but it may not be enough to completely snap you out of the sleep paralysis episode. Many still experience temporary paralysis upon waking. While waking somebody from a night terror might seem like the right and helpful thing to do, doing so usually doesn’t help. In fact, it may make the sleep paralysis worse, causing further disorientation, confusion, and fear.
How long does sleep paralysis last?
This will vary from person-to-person and episode-to-episode, but sleep paralysis usually only lasts a couple of minutes. Some only experience sleep paralysis for a couple of seconds. However, these episodes usually seem longer in our heads because we are still partly unconscious and dreaming.
Is sleep paralysis life-threatening?
While sleep paralysis is certainly scary, it is not life-threatening. What’s more life-threatening is sleep deprivation, which can stem from disturbed sleep caused by these episodes. If sleep paralysis is impeding your nightly rest and causing chronic daytime fatigue, you should talk with your doctor about possible solutions for easing stress and getting better rest.
Conclusion
Some people may experience an episode of sleep paralysis once in their lifetime. One incident isn’t a cause for worry. Getting better sleep and practicing good sleep hygiene prevents the sleep disorder from recurring; however, if this condition happens often, a physician can diagnose the underlying cause and get you the treatment you need.
About the author
Andrea Strand is a Certified Sleep Science Coach. She earned her Bachelor of Arts degree from Brigham Young University-Idaho where she studied English with an emphasis in Technical Writing. Since 2019, Andrea has written over 90 blog posts and guides on sleep health, sleep hygiene, and product reviews.
:max_bytes(150000):strip_icc()/BrandonPetersMD_1000-5143e542c3084368b1220c4b86ede01c.png)
:max_bytes(150000):strip_icc()/sanja-jelic-59517a7fa00c18165e7d8154.jpg)
:max_bytes(150000):strip_icc()/what-causes-sleep-paralysis-3014700_FINAL-b1afc63ebd504b5d9b8a67533cef21e7.png)
:max_bytes(150000):strip_icc()/Caitilin-Kelly_1000-51fc24dc524d4e00b4208047363fd064.jpg)
:max_bytes(150000):strip_icc()/Kashif-JPiracha-1000-ee93f3e24a26420d924b773aa0c6a6ea.jpg)